Palliative Massage: Key Benefits & How to Use in End‑of‑Life Care
 Oct, 20 2025
Oct, 20 2025
Palliative Massage Session Planner
Patient Condition Assessment
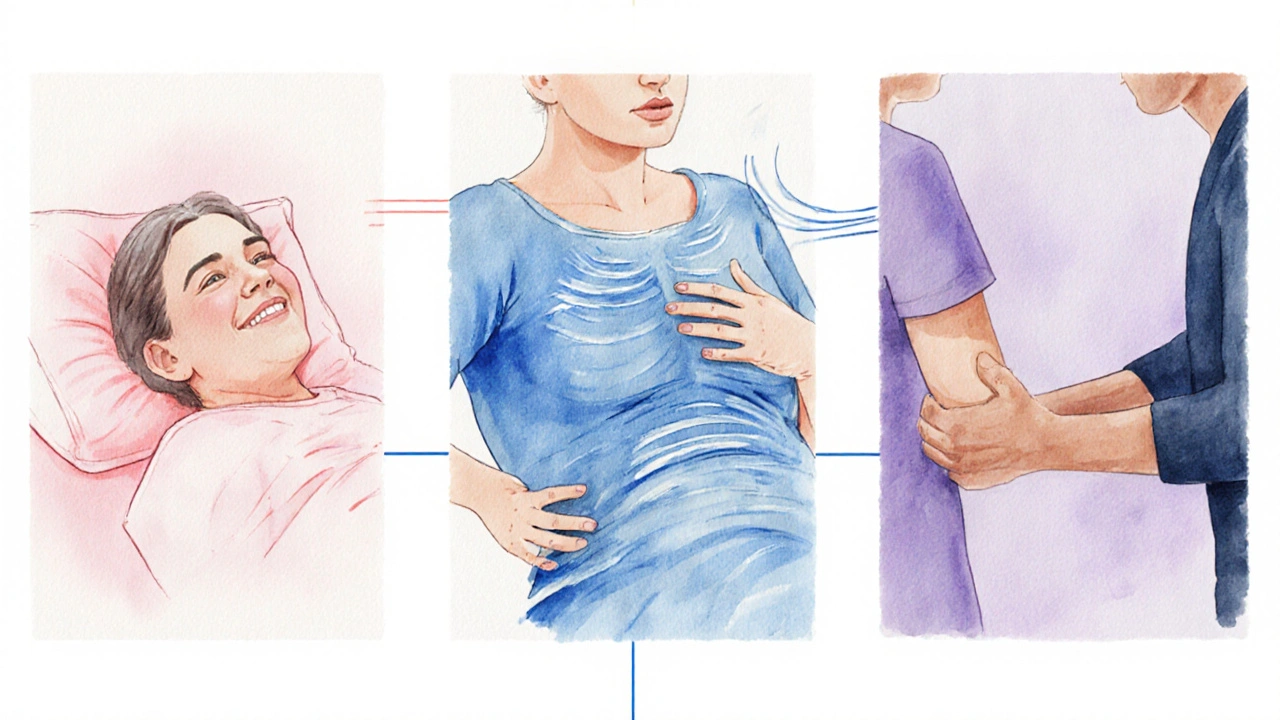
When caring for someone in the final stages of life, Palliative Massage is a gentle, therapeutic touch technique designed to ease discomfort, reduce anxiety, and improve overall quality of life for patients receiving palliative care. It isn’t about luxury; it’s about real, measurable relief when every moment counts.
What Exactly Is Palliative Massage?
In plain terms, palliative massage is a specialized form of bodywork that focuses on symptom management rather than on muscle conditioning or athletic performance. The goal is to address pain, breathlessness, insomnia, and emotional distress through light, adaptive strokes. Unlike a sports massage that pushes deep into tissue, this approach uses the smallest amount of pressure required to provoke a soothing response.
How It Differs From Regular Massage - A Quick Comparison
| Aspect | Palliative Massage | Traditional Massage |
|---|---|---|
| Primary Goal | Symptom relief & emotional comfort | Performance enhancement & injury prevention |
| Pressure Level | Light to moderate, always patient‑controlled | Varies from light to deep tissue |
| Typical Session Length | 15-30 minutes | 45-90 minutes |
| Setting | Hospice, hospital ward, home care | Spas, gyms, private clinics |
| Documentation | Detailed symptom tracking, interdisciplinary notes | Usually client‑focused progress notes |
Core Benefits for Patients and Families
- Pain reduction: Light stroking stimulates the release of endorphins, which can lower perceived pain scores by up to 30% in hospice studies.
- Improved breathing: Gentle rhythmic motions on the back and shoulders help relax the diaphragm, easing shortness of breath.
- Better sleep: The calming effect on the nervous system often translates into deeper, more restorative sleep.
- Emotional connection: Touch restores a sense of dignity and belonging, reducing feelings of isolation for both patients and caregivers.
- Family involvement: Training a family member to provide simple strokes empowers them and eases caregiver stress.
Getting Started - Training, Qualifications, and Safety
Before you can offer palliative massage, you need a solid foundation in both general massage therapy and the specific nuances of end‑of‑life care. Most credentialing bodies, such as the American Massage Therapy Association (AMA), recommend a minimum of 30 hours of palliative‑specific coursework. Key topics include:
- Recognizing contraindications (e.g., recent surgery, severe bruising).
- Understanding common medications and how they affect skin integrity.
- Communication skills for discussing goals with patients, families, and the palliative‑care team.
- Documentation standards set by the National Hospice and Palliative Care Organization (NHPCO).
Safety is non‑negotiable. Always check vital signs, watch for signs of discomfort, and maintain a clean, quiet environment. In Australia, the Australian Physiotherapy Association notes that even a light touch can alter blood pressure in frail patients, so regular monitoring is essential.
Integrating Into a Multidisciplinary Palliative Team
Hospice and palliative care thrive on collaboration. Your role as a massage therapist is to feed into the broader symptom‑management plan. A typical workflow looks like this:
- Attend the weekly case‑review meeting with doctors, nurses, social workers, and chaplains.
- Record observations using the World Health Organization (WHO) palliative‑care outcome checklist.
- Adjust your technique based on feedback - for example, focusing more on the hands if a patient reports increased nausea.
- Share a concise progress note with the team, highlighting changes in pain scores or mood.
This loop ensures that the massage isn’t an isolated activity but a measurable part of the patient’s overall comfort plan.
Practical Techniques You Can Use Today
Below are three widely accepted methods that work well in hospice rooms, home settings, and even bedside chairs:
- Effleurage with a feather‑light glide: Move your hands from the shoulders down the arms in slow, overlapping strokes. The goal is a soothing pressure that never triggers a pain response.
- Gentle joint mobilization: Very softly flex and extend the fingers or toes to maintain range of motion without stressing joints.
- Aromatherapy integration: A few drops of lavender or eucalyptus oil (if not contraindicated) can amplify the relaxation response.
Always ask the patient for a simple “yes/no” cue before each movement. A quick “Do you feel comfortable?” can prevent inadvertent overstimulation.

Common Myths & Pitfalls to Avoid
Myth #1: “Massage will cure pain.” Reality - it’s an adjunct, not a stand‑alone treatment.
Myth #2: “You need a fancy massage table.” Reality - a sturdy chair or hospital bed works fine as long as the patient feels safe.
Pitfall: Forgetting to document. In hospice, each session contributes to the patient’s care plan, and missing notes can lead to duplicated efforts or missed alerts.
Resources, Guidelines, and Where to Learn More
Here are a few reputable sources you can dive into for deeper knowledge:
- World Health Organization - “Palliative Care: Core Components” (2023 edition).
- National Hospice and Palliative Care Organization - Clinical guidelines for non‑pharmacologic symptom management.
- Australian Palliative Care Clinical Guidelines - Chapter on complementary therapies.
- Local workshops in Brisbane hosted by the Queensland Health Palliative Care Unit.
Enrolling in one of these programs not only boosts your skill set but also signals credibility to the healthcare team.
Quick Takeaways
- Palliative massage targets symptom relief, not performance.
- Light pressure, short sessions, and clear documentation are essential.
- Training via recognized bodies like AMA or NHPCO is a must.
- Integrate with the multidisciplinary team for measurable impact.
- Use simple techniques - effleurage, joint mobilization, aromatherapy - to start right away.
Is palliative massage safe for patients with cancer?
Yes, when performed by a therapist trained in oncology‑specific considerations. The therapist should avoid deep tissue work over tumor sites, watch for skin fragility, and coordinate with the oncology team for any medication‑related skin changes.
Can family members learn to give palliative massage?
Absolutely. Short, guided workshops teach gentle strokes that families can use to comfort their loved ones. The key is keeping pressure light, using simple cues, and respecting the patient’s comfort level.
How often should a patient receive palliative massage?
Frequency varies with individual needs. Many hospice programs schedule 2-3 sessions per week, while home‑care settings might offer daily short touch sessions if the patient enjoys them.
What documentation is required after each session?
A brief note covering: date, duration, pressure level, observed changes in pain or mood, patient’s verbal feedback, and any adjustments planned for the next visit.
Are there any contraindications I should watch for?
Yes. Avoid massage over open wounds, recent surgical sites, severe thrombocytopenia, or areas of active infection. Always check with the medical team before starting.